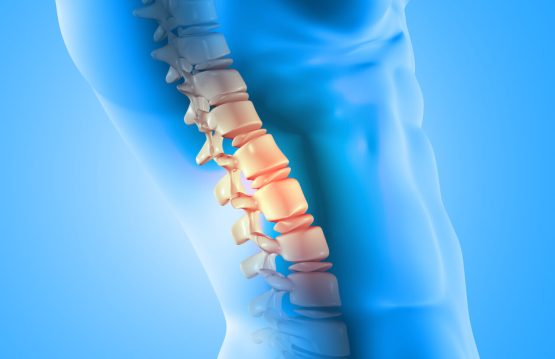
There are spinal infections that can affect the intervertebral discs. When it invades the vertebral plates (the cartilaginous structures that separate the intervertebral disc from the adjacent bone structure) and the vertebral bodies. they are called vertebral osteomyelitis.
If at the time of diagnosis the infection has already compromised 2 structures, it refers to spondylodiscitis. Moreover, this makes the purulent secretion can reach the epidural space (the space around the epidural sac – it is like a sac of tissue, made of dura mater), which causes the spinal cord/its last nerve fibers), causing a spinal epidural abscess.
CONTENT:
- What are the causes and factors that predispose to spinal infections?
- Symptoms
- Evolution and prognosis
- Diagnostic
- Treatment
What are the causes and factors that predispose to spinal infections?
- Diabetes
- Immunocompromised patients (also, organ transplant patients who are being treated with immunosuppressive drugs and intravenous drug users)
- Alcohol abuse
- Background surgery on the spine
- Neoplastic diseases (cancer)
- Rheumatic diseases
- Liver cirrhosis
- Renal insufficiency
- Minimally invasive non-surgical epidural procedures
Symptoms
At the clinical examination:
- Additionally, in children, loss of lumbar lordosis, fever, and neurological signs (muscle weakness, paresis, gait disorders) are most common.
- Adults report local pain in the back – neck / neck, associated with fever and may have neurological deficits – muscle weakness in the legs, urinary incontinence
- There is a clinical triad for spinal epidural abscess
1. Back pain
2. Fever
3. Neurological deficits (muscle weakness, paresis, sphincter disorders – urinary retention) - Paravertebral muscle contracture
- Root pain (pain that has the path of a nerve)
- Stiff neck (patient cannot bring chin to chest)
Evolution and prognosis
The unfavorable prognosis in cases of spinal cord infection is associated with:
- The advanced age of the patient
- The infection is located in the cervical / thoracic segment of the spine
- The presence of diabetes
- Heart disease
- Neurological disorders (muscle weakness, paresis) that have occurred for more than 36 hours
- Late diagnosis
- Infections with bacteria resistant to usual antibiotic treatment
Diagnostic
- With the help of inflammatory markers analyzed in the blood collected from the patient:
1. Red blood cell sedimentation rate (ESR)
2. C-reactive protein level (PCR)
3. The number of leukocytes - Bacteriological cultures of blood and urine collected from the patient
- Wound culture that has clinical signs of infection
- Imagistic:
1. Standard radiography: fast, easy to perform, but has the disadvantage that it does not provide clear evidence in the case of an isolated epidural abscess and does not reveal information about an osteomyelitis in the early stages.
2. Computed tomography (CT): highlights bone changes caused by an infection, pathological calcifications suggestive of bone tuberculosis.
3. Contrast-enhanced nuclear magnetic resonance imaging (MRI): Moreover, is the investigation of electives, having a great ability to provide information about the local anatomy, the extent of infection, destruction of adjacent tissues, and possible compression of the spinal cord.
Treatment
NON-SURGICAL TREATMENT
The indication for surgery in patients with spinal infection and neurological impairment (muscle weakness, paresis, sphincter disorders) is not questioned, but there are controversies regarding the choice of treatment for patients with minimal or even without neurological changes.
You can opt for treatment with antibiotics, to which bacteria are sensitive—an aspect established after a previous antibiogram was performed—combined with external immobilization or surgery. Additionally, this depends on the neurological status of the patient at presentation, the severity of the disease, the extent of tissue destruction adjacent, and antibiotic response.
SURGICAL TREATMENT
Surgery is performed immediately if there are signs of compression on the spinal nerves or spinal cord. Moreover, the operation should be considered if there is local pain (back / neck) or in case of changes in the curves of the spine, after non-surgical treatment.
The purpose of surgery is:
- Additionally, aggressive debridement of tissues affected by infection
- Collection of biological material for bacteriological examinations
- Decompression of spinal nerves and spinal cord
- Drainage of purulent collections from neighboring structures of the spine