Preventing osteoporosis is an essential component of general health care. This gives us the opportunity to build and maintain a strong and durable bone structure throughout our lives. Bones are the framework that supports our body, and to ensure that this foundation remains strong, we must pay special attention to preventive measures.
Osteoporosis is a common bone condition that particularly affects older people, but it can affect anyone. It is important to pay attention to your bone health from an early age to prevent the risk of developing osteoporosis throughout your life. In this article, we’ll explore essential information about osteoporosis prevention and ways you can keep your bones healthy.
CONTENT:
- The Importance of Healthy Bones for Preventing Osteoporosis
- Risk Factors for Osteoporosis
- Food Rich in Calcium and Vitamin D
- Regular physical exercises for the preventing osteoporosis
- Bone Health Monitoring through Medical Consultations
The Importance of Healthy Bones for Preventing Osteoporosis
The importance of healthy bones within our body is deeply rooted in the fundamental support of life and vital functions. Bones, as the basic element of the skeleton, perform a variety of crucial roles that contribute to the proper functioning of the entire body.
First, bones provide the structure and strength needed to support the entire body. This skeletal structure is not just a static frame; it participates in supporting movements, maintaining posture and providing the necessary stability for all our daily activities. Without a solid skeleton, the proper functioning of the body would be severely impaired.
Another essential function of bones is to protect delicate internal organs. The skull, spine, and ribs are examples of bony structures that act as a protective barrier for the brain, spinal cord, lungs, and other vital organs. Bones thus provide a protective shield against trauma and injury that could affect the internal system.
Bones also play a significant role in blood production. Bone marrow, found inside the bones, is responsible for the production of blood cells such as red blood cells, white blood cells, and platelets. These blood cells are essential for carrying oxygen, fighting infection and stopping bleeding, underscoring the importance of bone health for the efficient functioning of the circulatory system.
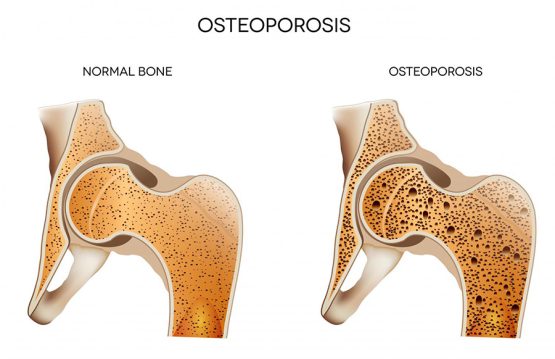
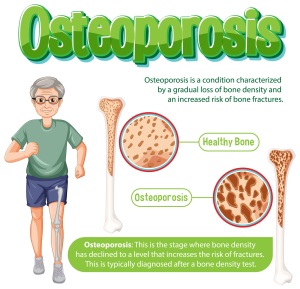
In the context of osteoporosis, it is vital to focus on bone density and bone quality. Osteoporosis affects these aspects, causing a gradual loss of bone density and increased bone fragility. This vulnerability to fractures and other complications becomes a major concern for the overall health of the individual.
Risk Factors for Osteoporosis
There are certain factors that can increase the likelihood of developing osteoporosis, including older age, female gender, family history, low levels of sex hormones, a diet low in calcium and vitamin D, smoking, and excessive alcohol consumption. The identification of these risk factors is crucial for the implementation of preventive measures.
Food Rich in Calcium and Vitamin D
Calcium and vitamin D are a pair of essential nutrients with a crucial role in maintaining bone health. These two compounds work in symbiosis to ensure optimal bone density and prevent the risk of osteoporosis.
1. Calcium – The Solid Foundation of Bones
Calcium is the main mineral involved in the formation and maintenance of bone structure. More than 99% of calcium in the body is found in bones and teeth, giving them the strength they need. A diet rich in calcium is crucial for ensuring the intake needed for bone maintenance. Excellent sources of calcium include:
- Dairy products: Milk, yogurt and cheese are rich sources of easily assimilable calcium. Choose low-fat options for a healthy intake.
- Green Leafy Vegetables: Broccoli, kale, spinach and other green leafy vegetables provide calcium and other essential nutrients.
- Nuts and Seeds: Almonds, sesame seeds and chia seeds are good sources of calcium, while also providing healthy fats and other beneficial nutrients.
- Fish: Certain types of fish, such as salmon and sardines, are an excellent source of calcium.
2. Vitamin D – The Bright Source for Healthy Bones
Vitamin D is essential for the efficient absorption and use of calcium in the body. This vitamin can be synthesized in the skin under the influence of sunlight, and an adequate level of sun exposure is crucial to ensure optimal production of vitamin D. Sources of vitamin D include:
- Sun Exposure: Spending time outdoors during the day, especially during sunny periods, stimulates the skin’s natural production of vitamin D.
- Fatty Fish: Salmon, tuna and sardines are not only good sources of calcium, but also of vitamin D.
Regular physical exercises for preventing osteoporosis
Regular physical activity is an essential component in promoting bone health and preventing osteoporosis. This practice not only strengthens the bone structure, but also contributes to the maintenance of general health and vitality. Next, we’ll explore the ways in which regular exercise becomes an important ally in maintaining bone health.
-
Swimming – Low Impact Physical Activity
Swimming is an excellent option for those looking for a physical activity with little impact on the joints, but which still offers considerable benefits for bone health. During swimming, all muscle groups are engaged, and the movements in the water provide resistance, helping to strengthen the bones without exposing the body to impact stress.
-
Weight Training – Building Bone Mass
Weight training, such as lifting weights or barbell exercises, are effective ways to build muscle mass and thereby stimulate bone density. These exercises stress the bones in a controlled and progressive way, improving their strength and functionality.
-
Variation and Consistency – The Keys to Success
To maximize the benefits of exercise on bone health, it is important to take a varied approach and maintain consistency in our fitness program. Combining low-impact and high-intensity activities, as well as alternating between cardio and strength training, contributes to a complex stimulus for bone remodeling.
Bone Health Monitoring through Medical Consultations
Regular doctor visits are essential for monitoring bone health and early detection of potential problems. Bone density tests offer crucial insights into bone health, guiding decisions for osteoporosis prevention or treatment.