Tests for Ankylosing Spondylitis are an essential pillar, providing valuable information for the early identification of the disease.
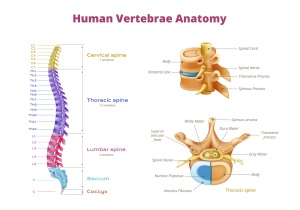
Ankylosing spondylitis is a chronic inflammatory condition primarily affecting the spine and sacroiliac joints, with insidious symptoms. In this context, the exploration of various tests and their role in the detection of ankylosing spondylitis becomes crucial. It is also important for the complete understanding of the process of diagnosis and management of this condition.
Through such investigations, specialists establish a personalized approach, providing patients a significant chance in battling this chronic disease.
CONTENT:
- Are there specific symptoms of Ankylosing Spondylitis?
- What are the tests for Ankylosing Spondylitis?
- Is there a test to confirm ankylosing spondylitis?
Are there specific symptoms of Ankylosing Spondylitis?
Yes, ankylosing spondylitis (AS) has specific symptoms. Recognizing them is essential for early diagnosis and effective management of the condition. Characteristic symptoms include:
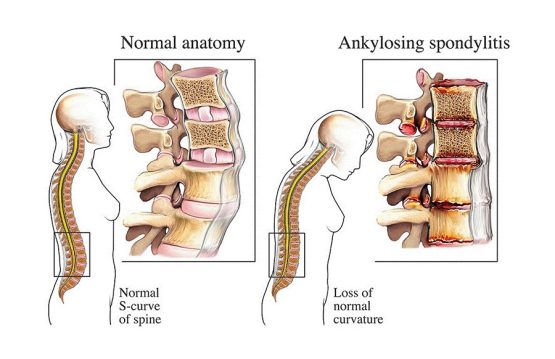
- Pain and stiffness: Persistent lower back pain is one of the main symptoms of ankylosing spondylitis. This pain may start gradually and become more intense over time. Spinal stiffness, especially in the morning or after long periods of inactivity, is also common.
- Reduced mobility: Patients with AS may experience a progressive loss of spinal flexibility. This can affect the ability to make large movements, such as bending or turning the body.
- Fatigue: Many patients with ankylosing spondylitis report chronic fatigue and loss of energy. This fatigue does not always correlate with physical activity and may persist even after adequate rest.
- Inflammation of the sacroiliac joints: Ankylosing spondylitis often affects the sacroiliac joints. Those are located at the bottom of the spine. Inflammation in this area can cause pain and stiffness in the lower back and buttocks.
- Extra-articular symptoms: In some cases, ankylosing spondylitis can also affect other joints in the body, as well as other organs, such as the eyes or lungs. These extra-articular symptoms may include eye inflammation (uveitis) or breathing difficulties.
- Presence of the HLA-B27 genetic marker: While not a symptom itself, ankylosing spondylitis is often associated with the HLA-B27 genetic marker, which can strengthen the diagnosis in combination with clinical symptoms.
What are the tests for Ankylosing Spondylitis?
Diagnosing ankylosing spondylitis involves a series of tests and investigations, which may include blood tests, medical imaging, and clinical evaluation. Here are some of the common tests and procedures used to diagnose ankylosing spondylitis:
1. Blood Tests
- HLA-B27:Doctors commonly use a blood test to detect the HLA-B27 genetic marker in diagnosing ankylosing spondylitis. However, the presence of this marker does not necessarily confirm the diagnosis and may also be present in other conditions.
- C-reactive protein (CRP) and ESR (Erythrocyte Sedimentation Rate): Measuring these markers provides information about the elevated inflammation often seen in ankylosing spondylitis.
- Antibody level: Other tests may include measuring specific antibodies, such as anti-CCP (cyclic citrullinated peptide) antibodies, which may be present in other rheumatologic diseases but are not specific for ankylosing spondylitis.
2. Medical Imaging
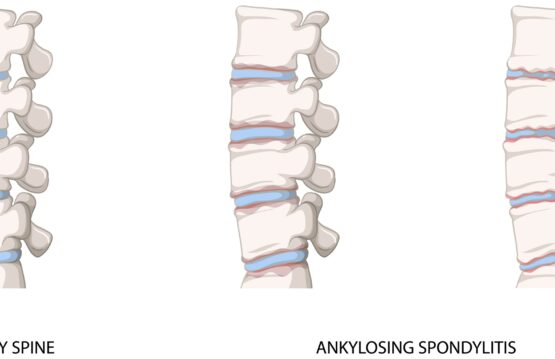
- X-rays: X-rays of the spine and sacroiliac joints may show characteristic changes such as bone erosions and the formation of new bone tissue (osteoproliferation).
- Magnetic Resonance Imaging (MRI): is very useful for detailed visualization of the spine and sacroiliac joints, highlighting inflammation and soft tissue damage.
- Computed Tomography (CT): can be used to obtain detailed images of joints and bones, especially to assess bone changes.
3. Differential diagnosis
The doctor can use information from blood tests and medical imaging to rule out other conditions that may have similar symptoms, such as rheumatoid arthritis or other types of spondyloarthropathies.
4. Clinical Evaluation
- Medical history and physical exam: The doctor will consider the patient’s medical history, including reported symptoms, and perform a physical exam to identify signs specific to ankylosing spondylitis, such as limited spinal mobility.
- Functional imaging: Techniques such as bone scintigraphy or X-ray imaging may be used to assess joint function and identify areas of inflammation or increased bone activity.
It is important to emphasize that an accurate diagnosis is made by combining the information obtained from these tests and procedures, as well as by consulting a specialist, usually a rheumatologist. If you have symptoms suggestive of ankylosing spondylitis, it is crucial to seek medical attention for proper evaluation and accurate diagnosis.

Is there a test to confirm ankylosing spondylitis?
There is no single test that can definitively confirm ankylosing spondylitis. The diagnosis of this rheumatologic condition is based on a combination of blood tests, medical imaging, medical history, physical examination, and clinical evaluation performed by a medical specialist, usually a rheumatologist.
However, there are specific tests and markers that can support the diagnosis and help guide the doctor in the evaluation process.