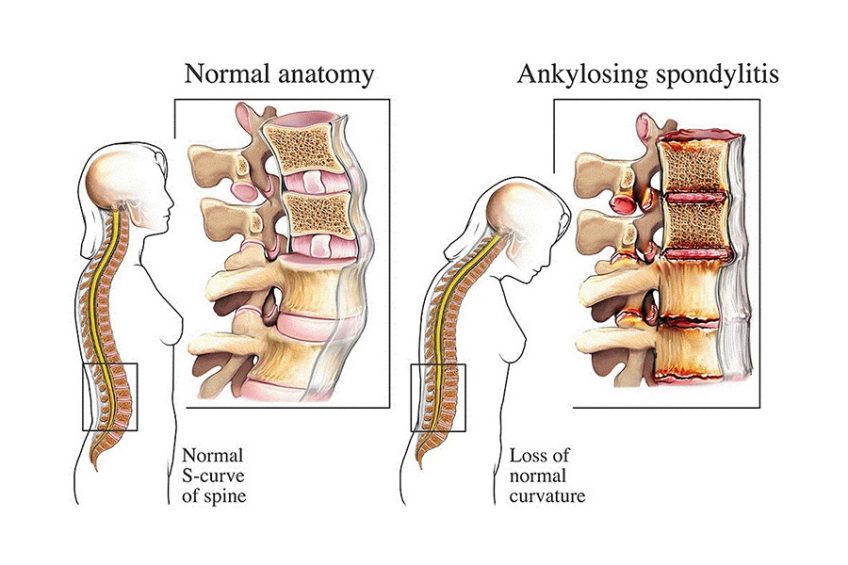
Ankylosing spondylitis is an inflammatory disease that involves the fusion of certain vertebrae that form the spine, a process that leads to stiffening of the spine and the development of a hunchbacked posture, as well as respiratory difficulties, especially if the vertebrae in the rib cage are affected. According to statistics, men are more likely to develop this condition. Even if it is not curable, certain medications and physiotherapy help to relieve the symptoms of ankylosing spondylitis and can slow its progression.
As we age, the spine, which bears much of the effort we make every day, undergoes transformations. Mainly, it loses its elasticity, it can no longer absorb the shocks felt, the intervertebral discs suffer various injuries (they lose water, break or deform).
Spondylitis (or spondyloarthritis, not to be confused with spondylosis) is a form of arthritis, a progressive chronic disease that causes inflammation in the spine and in the peripheral joints. Inflammation can be traumatic, infectious or tuberculous. When spondylitis affects the spine, the vertebrae fuse, leading to stiffness and limited mobility.
CONTENT:
Causes of Ankylosing Spondylitis
Ankylosing spondylitis may have a genetic component, but researchers have not yet well-determined the cause of this condition. According to experts, people who have the HLA-B27 gene have a higher risk of developing this condition. This is because the gene causes the immune system to respond excessively to the attack of certain bacteria in the body, which causes the inflammation that underlies the symptoms of ankylosing spondylitis.
A person is more likely to suffer from spondylitis if they have a family history of complications or other similar problems. Some elements associated with spondylitis include:
-
Previous inflammation in the joints and tissues, which can exacerbate similar problems caused by spondylitis
-
Lack of exercise
-
Obesity
-
Smoking or excessive alcohol use
-
Back problems such as degenerative disc disease or spinal stenosis
-
Hereditary factors and spondylitis

Spondylitis is considered a hereditary disease, although environmental factors are also involved. Most people with HLA-B27 antigen do not develop spondylitis. Men are affected four times more frequently than women in the case of spondylitis. The onset typically occurs between the ages of 15 and 45.
Genetics play a role, and the risk of developing spondylitis can increase if a family member is diagnosed with spondylitis or has a history of back pain or other common problems.
Spondylitis is thought to be genetically inherited, and most people with this condition (almost 90%) are born with a gene known as the HLA-B27 gene. Scientists developed blood tests to detect the HLA-B27 gene marker, aiding in understanding the relationship between HLA-B27 and spondylitis. The HLA-B27 gene appears only to increase the tendency to develop ankylosing spondylitis, while other factors, such as the environment, are required for the disease to occur or manifest.
For example, while 7% of the United States population has the HLA-B27 gene, only 1% of the population actually has ankylosing spondylitis. In northern Scandinavia (Lapland), 1.8% of the population has ankylosing spondylitis, while 24% of the general population has the HLA-B27 gene. Even among individuals with a positive HLA-B27 blood test, the inheritance of the risk of developing spondylitis still seems to occur. In HLA-B27 positive individuals with relatives affected by this disease, the risk of developing spondylitis is 12% (six times higher than for those whose relatives do not have spondylitis).
Symptoms of Ankylosing Spondylitis
The early symptoms of ankylosing spondylitis usually appear around the age of 45 and consist of pain and stiffness in the lower back and thighs, especially in the morning or after a period of rest or sitting. Sore throat and fatigue are also common symptoms of ankylosing spondylitis. Other manifestations of ankylosing spondylitis may be:
- Formation of an unsightly curve in the spine
- Pain or numbness in the shoulders, thighs, hands or even the Achilles tendon
- Swelling of the joints
- Difficulty breathing
- Pain during sneezing or coughing
- Gastrointestinal disorders (diarrhea, fecal blood, abdominal cramps)
- Depression and / or anxiety
- Eye inflammation (uveitis), blurred vision, sensitivity to light
- Cardiac arrhythmia
Ankylosing spondylitis treatment
Therapeutic management of ankylosing spondylitis includes general measures and specific drug treatment.
The goals of treatment are:
- reduction of inflammation and pain;
- maintaining mobility and joint function;
- prevention of the appearance of ankylosis at the level of the spine (slowing down the progression of radiological lesions and the appearance of ankylosis);
- minimizing extra-articular manifestations and peripheral damage;
- prevention of complications in the spine.
Drug treatment
It contains the following therapeutic solutions:
- NSAIDs;
- Analgesics;
- DMARDs;
- Corticosteroids;
- Biological anti-TNFα agents.
Non-pharmacological treatment
Education includes general principles such as:
- smoking avoidance (which contributes to pulmonary fibrosis);
- the patient will sleep on a hard bed, without a pillow under his head, in a prone position, to avoid vicious positions in flexion.
Physical therapy comprises a program of daily physical exercises to prevent spinal deformity and maintain chest expansion through respiratory gymnastics. We recommend hydrotherapy and swimming because they play a role in optimizing the effect of physical therapy. Physiotherapy includes administering electrotherapy sessions (interference currents, galvanic currents, TENS, ultrasound) with an adjuvant role, and doctors recommend them during periods of disease remission.
Occupational therapy aims to re-educate normal movements, complementing the results of physical therapy. It is the final method of adapting free muscles to the possibilities of professional recovery until the recovery of normal movements. There will be 2-3 sessions per week, their duration not exceeding 60-90 min. While applying these methods, we will correct static disorders of the spine and adopt positions that allow the intervertebral disc to rest.
The patient should refrain from carrying weights, avoid excessive movements and harmful positions, and adopt activity-friendly postures. Occupational therapy aims to return the patient to the basic profession. If this is not possible he will have to learn another trade. The methods prevent patients from becoming dependent, enabling them to contribute to society based on their abilities and inclinations.