Fibromyalgia depression is a complex and often difficult reality to manage. For those living with this chronic condition characterized by diffuse muscle pain and intense fatigue, the mental state can become as important as the physical manifestations of the disease. Scientific findings and patient experiences are increasingly highlighting the close connection between fibromyalgia and depression, giving us more insight into how these two entities interact and how we can manage our mental health in the context of this dual medical challenge.
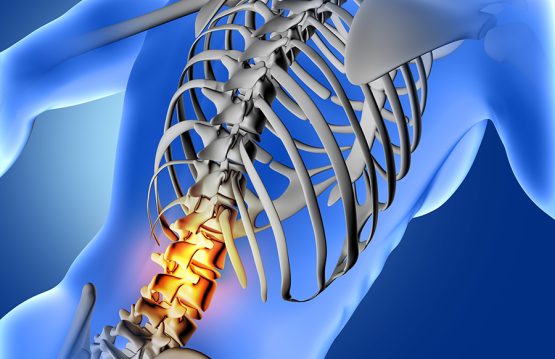
Fibromyalgia is a chronic condition characterized by diffuse muscle pain, intense fatigue and tender points in various areas of the body. This disease affects not only the body, but also the mental state of those living with it, which can lead to depression. In this article, we’ll explore the connection between fibromyalgia and depression, and how we can manage and improve our mental health in the face of this dual diagnosis.
CONTENT:
- Understanding the link between fibromyalgia and depression
- How depression manifests itself in the context of fibromyalgia
- Strategies for managing fibromyalgia depression
Understanding the link between fibromyalgia and depression
Fibromyalgia and depression intersect in a complex way, forming a connection that can profoundly affect patients’ quality of life. In light of recent research, it is increasingly evident that this association is not coincidental, but rather reflects a profound interaction between the physical and psychological aspects of this condition.
1. The Combined Impact of Chronic Pain and Mental Health
Fibromyalgia, characterized by diffuse muscle pain and tender points, creates a persistent physical burden. When this is associated with depression, the result can be an exacerbation of suffering. Chronic pain can negatively influence mood and contribute to a vicious cycle between physical discomfort and mental disorders.
2. Prevalence of Depressive Symptoms in Fibromyalgia
Studies show that between 30% and 40% of people diagnosed with fibromyalgia also develop symptoms of depression. This co-prevalence indicates that these two conditions may mutually influence their occurrence and evolution. Understanding this aspect becomes crucial for the holistic management of fibromyalgia patients.
3. Physical and Psychological Factors Involved
- Sleep Disorders: People with fibromyalgia often experience sleep disorders, such as insomnia or restless sleep. They can contribute to the onset and exacerbation of depressive symptoms, having a significant impact on quality of life.
- Chronic Stress: The constant pain and fatigue associated with fibromyalgia can induce chronic stress. Stress, in turn, can worsen depressive symptoms, creating a vicious cycle that can be difficult to break.
- Chemical Changes in the Brain: Some studies suggest that fibromyalgia may be associated with changes in neurotransmitters in the brain, such as serotonin and norepinephrine, the same chemicals involved in mood regulation. This chemical connection adds a complex dimension to understanding the link between fibromyalgia and depression.
Overall, it is evident that depression in the context of fibromyalgia is not just a simple coexistence, but an intricate interaction between the physical and psychological aspects of this condition. Adequately addressing this complex relationship requires a deep understanding of the factors involved and a holistic approach to effectively manage both the physical and psychological symptoms of fibromyalgia patients.

How depression manifests itself in the context of fibromyalgia
Depression associated with fibromyalgia brings with it a number of symptoms that can significantly influence the quality of life of patients. Recognizing and understanding these signs are crucial steps in fully addressing the complex impact of this dual diagnosis.
1. Persistent Sadness
Deep and persistent sadness is one of the core symptoms of depression in fibromyalgia. Patients may experience a general state of melancholy that is not directly related to difficult times, but becomes a constant presence in everyday life.
2. Loss of Pleasure in Usual Activities
Another defining aspect of depression associated with fibromyalgia is the loss of pleasure in activities that the patient normally enjoys. Activities that once brought joy and satisfaction may now become uninteresting and no longer generate the same pleasure.
3. Changes in Weight or Appetite
Depression can affect appetite and body weight. Patients may experience either increased or decreased appetite, leading to weight fluctuations. These changes can have a negative impact on your overall health and self-esteem.
4. Difficulty concentrating
Managing the chronic pain and physical symptoms of fibromyalgia can affect your ability to focus and pay attention. Depression exacerbates these difficulties, making daily and professional tasks more demanding and contributing to a sense of ineffectiveness.
5. Feelings of Hopelessness
Depression in fibromyalgia can bring with it strong feelings of despair and hopelessness. Patients may have difficulty anticipating improvement and may experience a general lack of perspective about their future.

Strategies for managing fibromyalgia depression
- Medical treatment and therapy: Consultation with a mental health specialist and a rheumatologist may be essential. Cognitive-behavioral therapies and antidepressant medications can provide support in managing symptoms.
- Regular physical exercise: Moderate physical activity can have a positive impact on fibromyalgia pain and improve mood. Consult a medical professional to choose appropriate exercises.
- Stress management and relaxation: Techniques such as meditation, yoga or deep breathing can help reduce stress and anxiety, contributing to improved mental health.
- Social support: Building a support system of friends, family, or support groups can provide an avenue for sharing experiences and finding solutions together.
Fibromyalgia depression can be a significant challenge, but approached with a well-structured plan and appropriate support, it can be managed. Each individual is unique, and personalized approaches will be most effective in managing the dual impact of this condition. Consulting with health professionals and implementing a holistic management plan can make significant improvements in the quality of life for affected individuals.