Rheumatoid arthritis (RA) is a chronic, inflammatory condition that affects the joints, causing pain, swelling and stiffness. It is important to better understand this disease in order to be able to manage the symptoms and ensure a better quality of life for those affected. In this article, we will explore ten essential aspects related to rheumatoid arthritis.
CONTENT:
- RA causes
- Symptoms of RA
- Early diagnosis
- The Role of Genetic Factors
- Personalized Treatment
- Impact on Quality of Life
- Systemic complications
- The Role of Physical Exercises
- Alternative and Complementary Medicine
- Future Perspectives
1. RA causes
The causes of rheumatoid arthritis (RA) are complex and involve a combination of genetic and environmental factors. A central aspect of this condition is its autoimmune nature, where the immune system, responsible for defending the body against infection, misdirects its attention to its own tissues.
In rheumatoid arthritis, the immune system mistakenly attacks the synovial membranes, which are the tissues that cover the joints. These membranes are essential for the proper functioning of the joints, facilitating their movement and ensuring proper lubrication. When the immune system attacks these membranes, the result is inflammation, swelling and joint damage.
Although the exact mechanism that triggers this autoimmune reaction is not yet fully understood, there are several factors that may contribute to the onset of rheumatoid arthritis. An important factor is genetic predisposition. People with certain genes may have a higher risk of developing RA, but this is not the only cause.
2. Symptoms of RA
The symptoms of rheumatoid arthritis (RA) are diverse and can vary depending on the severity of the disease and how it progresses over time. It is important to recognize and understand these symptoms in order to initiate the earliest and most effective treatment. Here is a more detailed development of the characteristic symptoms of rheumatoid arthritis:
-
Joint Pain
Joint pain is a central symptom of rheumatoid arthritis and can affect several joints simultaneously or at different times during the course of the disease. This pain can be felt as a tingling, throbbing or burning sensation, and its intensity can range from mild to severe. The pain may be worse in the morning or after periods of inactivity.
-
Joint Swelling
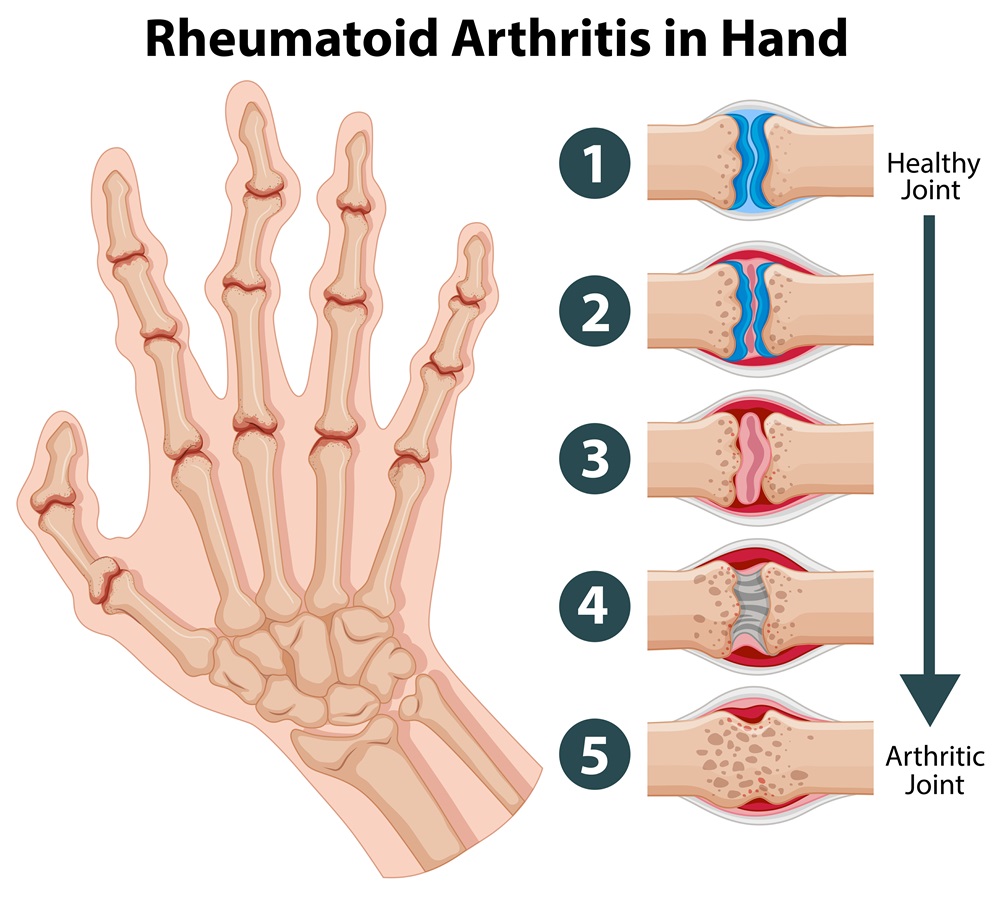
Joint swelling is the result of inflammation produced by the immune system in the synovial membranes. Affected joints become swollen, tender to the touch and can sometimes have a higher temperature than the rest of the body. Persistent swelling can lead to joint damage and deformities.
-
Joint Stiffness
Joint stiffness is another hallmark of rheumatoid arthritis. Patients may experience joint stiffness, especially in the morning or after periods of inactivity. This symptom may affect the ability to move and may last more than an hour.
-
Muscle Weakness
Rheumatoid arthritis can cause muscle weakness, and patients may experience a general feeling of fatigue and exhaustion. This weakness can occur both in the muscles near the affected joints and throughout the body.
-
Symmetric Affection
A distinctive feature of rheumatoid arthritis is symmetrical joint damage. This means that usually the same joints on both sides of the body are involved at the same time. For example, if a finger joint on the left hand is affected, the same joint on the right hand is likely to show similar symptoms.
-
Variability of Symptoms
Rheumatoid arthritis symptoms can vary in intensity and may come and go during periods called “flare-ups” and “remissions”. Flare-ups are periods when symptoms worsen, while remissions are periods when symptoms are milder or even absent.
3. Early diagnosis
Early diagnosis is an essential element in the effective treatment of rheumatoid arthritis (RA), having a significant impact on the prognosis and quality of life of patients. Here are some relevant points that emphasize the importance of early diagnosis in the management of rheumatoid arthritis:
-
Preventing Joint Damage
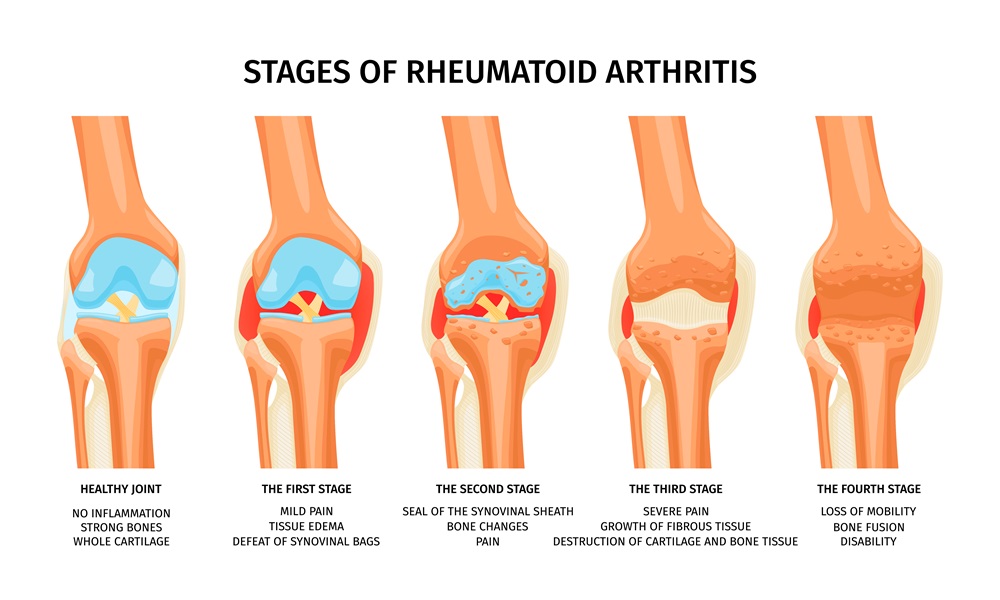
One of the main reasons early diagnosis is crucial in rheumatoid arthritis is the ability to prevent joint damage. In the early stages of the disease, prompt treatment can help control inflammation and slow down the process of joint tissue destruction. If rheumatoid arthritis is left untreated or is diagnosed at an advanced stage, irreversible damage to the joints can occur, which significantly affects the functionality and mobility of the patient.
-
Symptom Management and Quality of Life Improvement
Early diagnosis allows rapid initiation of an appropriate treatment plan, which can help control symptoms and improve the patient’s quality of life. Joint pain, swelling and stiffness can be managed more effectively with early therapeutic interventions, allowing the patient to maintain optimal joint function and lead as normal a life as possible.
-
Prevention of Systemic Complications
Rheumatoid arthritis doesn’t just affect the joints; it can also have systemic complications involving internal organs such as the heart, lungs, and blood vessels. Early diagnosis and appropriate management can help prevent these complications and maintain overall health.
-
Optimizing Treatment Response
Treatment of rheumatoid arthritis can vary depending on the stage of the disease and individual response to therapy. An early diagnosis gives the doctor the opportunity to more effectively adapt the treatment plan according to the specific needs of the patient and to optimize the management of the disease.
-
Patient Involvement in Therapeutic Decisions
Early diagnosis allows the patient to be more active in the decision-making process regarding treatment. Early understanding of the disease and treatment options gives the patient the opportunity to collaborate with the medical team in developing a personalized plan that aligns with their individual needs.
4. The Role of Genetic Factors
The role of genetic factors in the occurrence of rheumatoid arthritis (RA) is well established, and genetic predisposition is one of the main pillars of this autoimmune disease. However, it is important to emphasize that genetics is not the only determining factor in the development of AR, but interacts in a complex manner with environmental factors.
-
Genetic Predisposition
Studies have shown that there are certain genes associated with an increased risk of developing rheumatoid arthritis. HLA-DRB1 is an example of a gene with a strong link to AR. People who inherit certain variants of this gene have an increased risk of developing the disease. However, although genetic predisposition is important, not everyone who inherits these genes actually develops RA. Thus, environmental and other factors may intervene crucially.
-
Interaction with Environmental Factors
Even if a person has a genetic predisposition to RA, it is not an inevitable fate. Environmental factors, such as exposure to certain infections, smoking, stress and other lifestyle factors, can play an important role in triggering the disease in those with a genetic susceptibility. Infections, in particular, have been associated with the onset of rheumatoid arthritis in some cases, suggesting that they may activate the immune system and help initiate the autoimmune response.
-
The Complexity of Genetic and Environmental Interaction
The interplay between genetic and environmental factors in the occurrence of AR is complex and still not fully understood. It is believed that certain events or exposures in a person’s life can trigger abnormal immune reactions in those with a genetic predisposition. These incorrect immune reactions can cause the chronic inflammation characteristic of rheumatoid arthritis.
-
Importance of Risk Factor Assessment
Identifying the genetic and environmental factors associated with rheumatoid arthritis is essential to develop personalized prevention and treatment strategies. People with a family history of RA may benefit from closer monitoring and preventive interventions to minimize the risk of developing the disease.
5. Personalized Treatment
Management of rheumatoid arthritis usually involves a personalized approach. Anti-inflammatory medications, lifestyle changes, and physical therapy are just a few treatment options that can be customized to the individual patient’s needs.
6. Impact on Quality of Life
Rheumatoid arthritis can significantly affect the patient’s quality of life. Chronic pain and discomfort can lead to emotional disorders such as anxiety and depression. Emotional support and counseling can be essential in managing these issues.
7. Systemic complications
Rheumatoid arthritis (RA), in addition to its impact on the joints, can cause systemic complications, affecting internal organs and contributing to various conditions. Understanding these complications is crucial to ensure a complete and appropriate management of the disease.
-
Affecting the Cardiovascular System
Rheumatoid arthritis can increase the risk of cardiovascular disease. The chronic inflammation associated with RA can damage the artery wall, increasing the risk of atherosclerosis and blood clots. RA patients may also have a higher risk of heart disease and stroke. Blood pressure monitoring, cholesterol levels and prevention of cardiovascular risk factors thus become a priority.
-
Affecting the Respiratory System
The lungs can be affected in rheumatoid arthritis, causing complications such as pulmonary fibrosis, pleurisy or pneumonitis. These conditions can cause breathing difficulties and compromise the normal functioning of the lungs. Monitoring of respiratory function and periodic assessment of lung status are essential for early detection of these complications.
-
Affecting Blood Vessels
RA can affect blood vessels by causing vasculitis, an inflammation of the vessel wall. Vasculitis can affect various organs, including the skin, nerves, kidneys, and others. This complication can have serious consequences, and careful monitoring of the condition of the blood vessels is essential to prevent vascular complications.
-
Bone and Marrow Complications
Rheumatoid arthritis can contribute to bone loss and eventually osteoporosis. Weakened bones can increase the risk of fractures. Chronic inflammation can also affect the bone marrow, contributing to anemia or other hematological disorders. Bone density assessment and blood monitoring for abnormalities are necessary to prevent and manage these complications.
-
Eye Diseases
Rheumatoid arthritis can affect the eyes, leading to conditions such as Sjögren’s syndrome (an autoimmune disorder that affects the glands that produce tears and saliva) or scleritis (inflammation of the outer layer of the eye). Regular eye exams are essential for early detection and treatment of these problems.
8. The Role of Physical Exercises
Regular exercise can play a crucial role in managing the symptoms of rheumatoid arthritis. They can improve patients’ mobility, muscle strength and mood.
9.Alternative and Complementary Medicine
Certain complementary therapies, such as acupuncture, massage, and yoga, can provide relief for rheumatoid arthritis. However, it is important to always talk to your doctor before trying such treatments.
10. Future Perspectives
Rheumatoid arthritis research is ongoing, and new therapies and approaches may bring hope for patients in the future. Involvement in clinical trials and maintaining open communication with the medical team can contribute to more effective disease management.