Rheumatic pain, these unpleasant companions of everyday life, often become the protagonists of the autumn landscape. As the seasons change, many rheumatic sufferers experience an increase in symptoms, turning the chilly days into additional challenges for their well-being.
It is as if nature itself plays a role in this drama of lingering pain, and those affected seek answers to the question of why autumn often becomes their unexpected accomplice. In this review, we’ll explore the mystery behind worsening rheumatic pain this time of year and offer insights into management strategies that can bring relief in the fight against joint discomfort.
CONTENT:
- Meteorological factors and impact on rheumatic pain
- Immunity and the cold season
- Strategies for managing rheumatic pain in the fall weather
Meteorological factors and impact on rheumatic pain
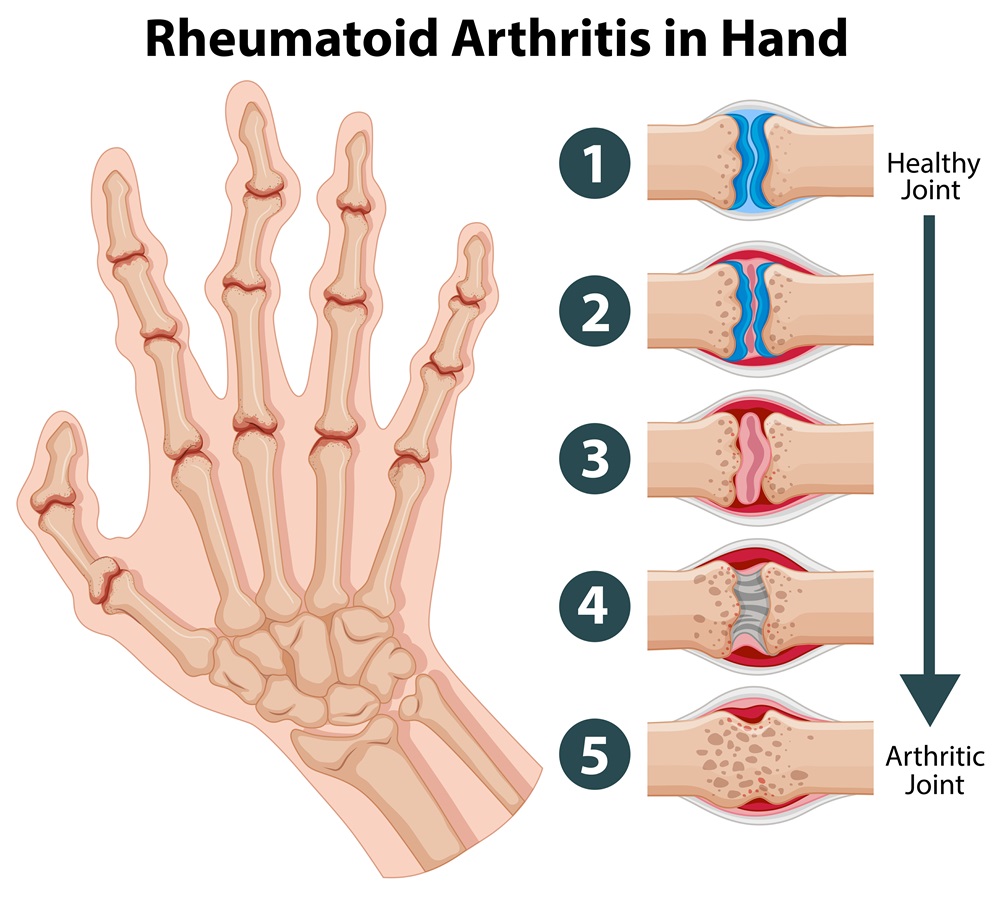
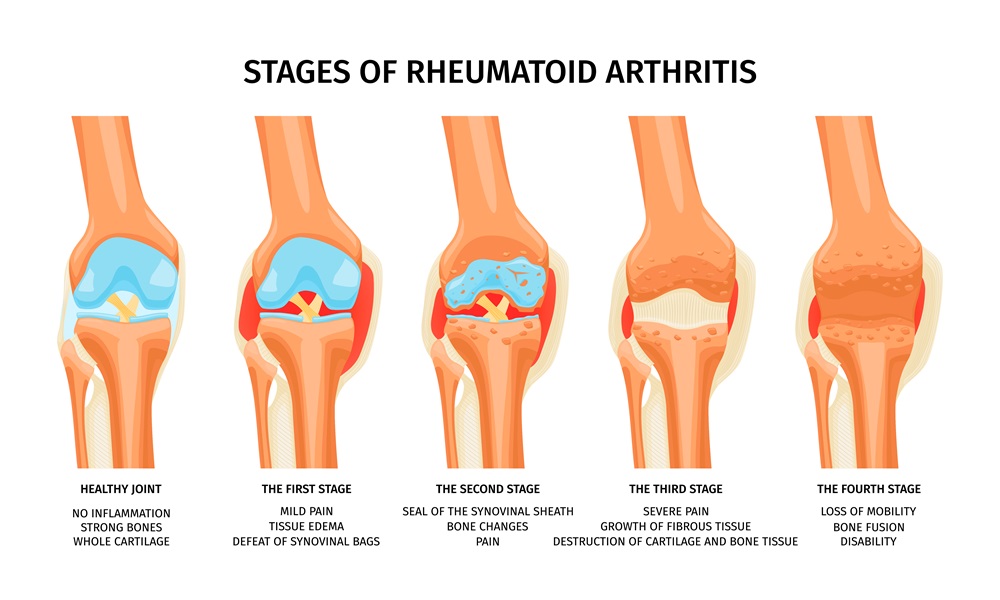
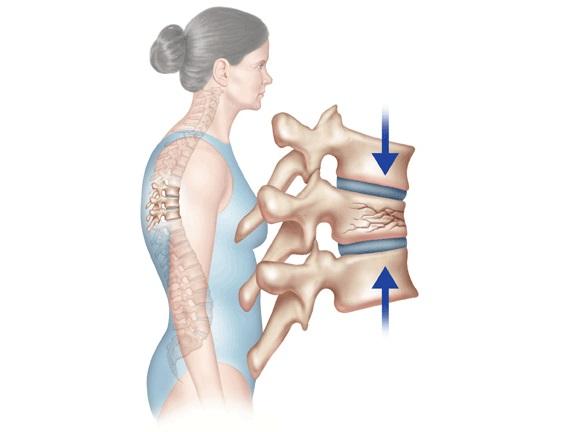
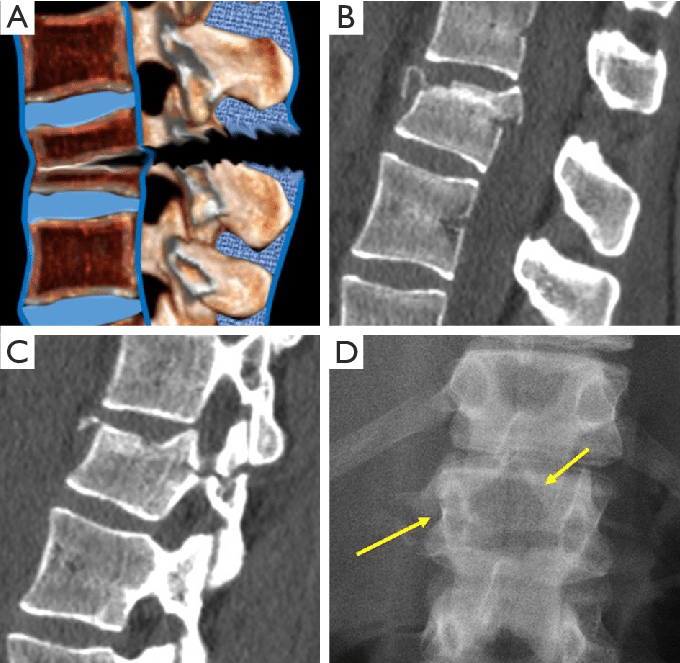
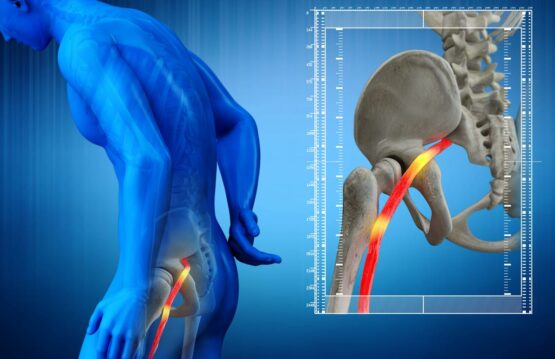
One of the main factors contributing to the worsening of rheumatic pains in autumn is the change in weather conditions. Lower temperatures, increased humidity and changes in atmospheric pressure can affect joints and the tissues around them. Patients with rheumatic conditions such as rheumatoid arthritis or osteoarthritis may experience increased stiffness and discomfort in cold, wet weather.
Atmospheric pressure can also affect the connective tissues and fluids in the joints, contributing to inflammation and pain. Studies have shown that sudden changes in temperature and atmospheric pressure can be associated with the intensification of rheumatic symptoms, although the exact mechanisms are still the subject of research.
Immunity and the cold season
Immunity and the cold season play a key role in understanding the worsening of rheumatic pain in autumn. With the arrival of colder temperatures, respiratory infections, such as flu and colds, become more common, creating an environment conducive to the onset or intensification of symptoms in people with rheumatic conditions.
People affected by rheumatism can often have an increased vulnerability of the immune system, which makes them more susceptible to infections. Fighting these infections can become an additional challenge, with direct consequences on their joint health. Infections can activate the body’s inflammatory mechanisms, increasing pain and stiffness around the joints.
Managing overall health during the cold season therefore becomes crucial for those affected by rheumatism. Avoiding contact with sick people, rigorous hand hygiene and compliance with preventive measures, such as flu vaccination, are important steps to reduce the risk of contracting respiratory infections. A healthy lifestyle, characterized by a balanced diet, moderate exercise and adequate rest, can help maintain a robust immune system and, implicitly, reduce the impact of infections on rheumatic symptoms.
Strategies for managing rheumatic pain in the fall weather
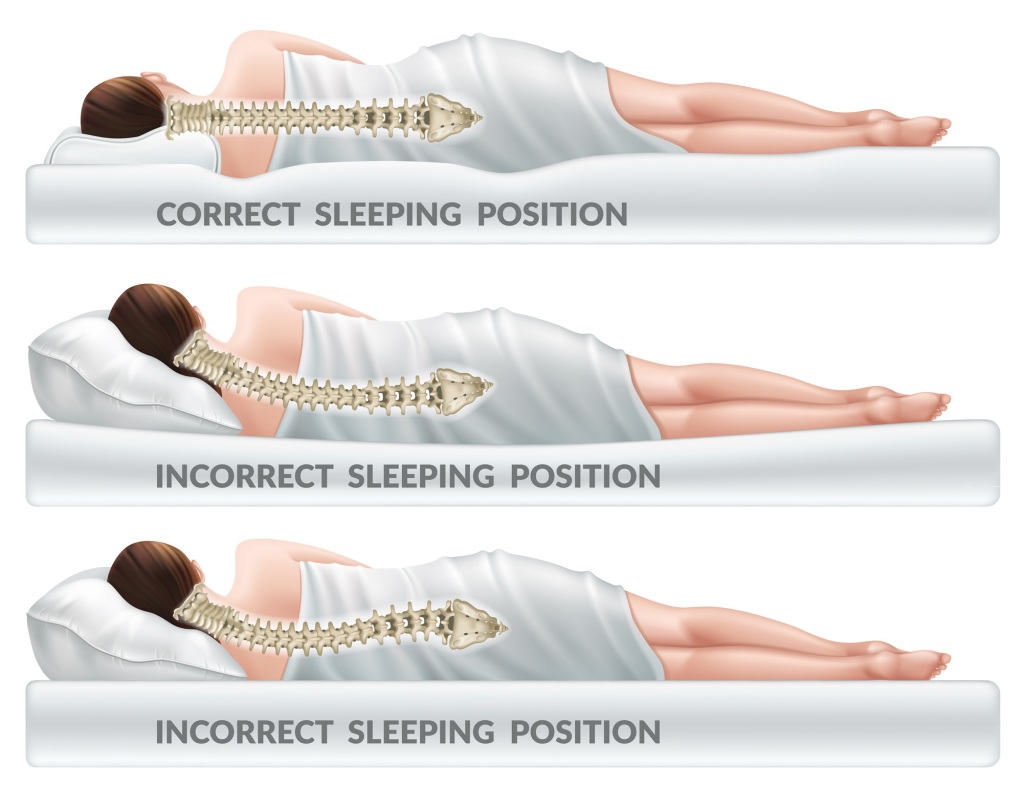
1. Keeping warm
Maintaining an optimal body temperature is essential in the effort to reduce joint stiffness. Selecting appropriate clothing and using thermal blankets in cold weather can effectively shield the joints, offering additional protection.
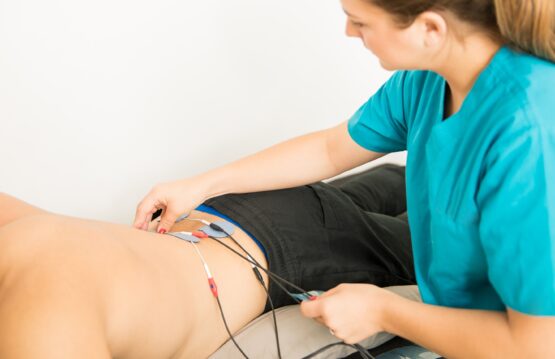
2. Moderate physical activity
Regular exercise is an essential pillar in maintaining joint health. A moderate physical activity routine can help maintain joint flexibility and strength. Consultation with a physiotherapist can help develop a personalized program tailored to individual needs and specific limitations.
3. Anti-inflammatory diet
Diet plays a crucial role in managing the inflammation associated with rheumatic pain. Including foods rich in omega-3 fatty acids, antioxidants and vitamins in the diet can have anti-inflammatory effects. Fatty fish, flax seeds and a variety of colorful fruits and vegetables should be essential components of a balanced diet.
4. Stress Management
Stress can exacerbate rheumatic symptoms, so it is crucial to adopt relaxation techniques. Yoga, meditation and other similar practices can significantly contribute to reducing stress levels, having a positive impact on pain.

Adopting these strategies offers a holistic approach to managing fall-related rheumatic pain, emphasizing the need for ongoing care for both body and mind.
Although the relationship between fall and worsening rheumatic pain is complex and not fully understood, there are strategies patients can adopt to more effectively manage this difficult time. Seeking specialized medical advice and adopting a holistic health approach can significantly enhance the quality of life for those grappling with these conditions.